A duodenal ulcer is a sore on the lining of the duodenum, the first part of the small intestine, often caused by the H. pylori bacteria or long-term use of NSAIDs. Common symptoms include a burning or gnawing stomach pain, bloating, nausea, and feeling full quickly. Treatment focuses on eliminating the cause through medication, such as antibiotics and acid-reducing drugs, and potentially making lifestyle changes
Duodenal ulcer

Here’s a comprehensive overview of duodenal ulcers — causes, symptoms, diagnosis, treatment, complications, prevention and special-cases. This is for general educational purposes only; always consult a healthcare provider for individual advice.
What is a duodenal ulcer?
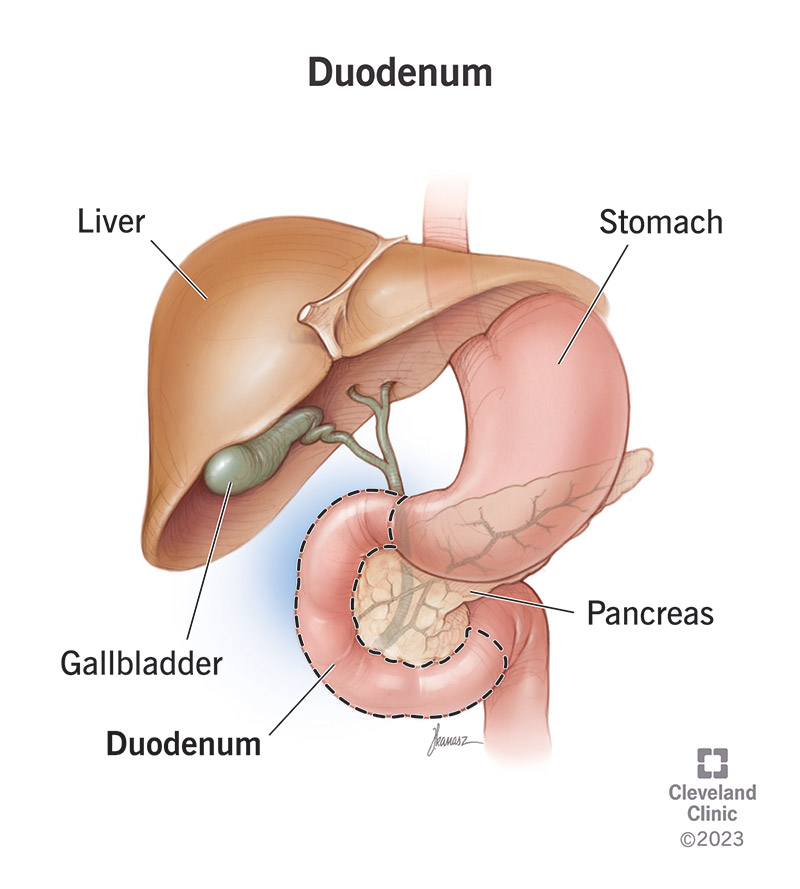
A duodenal ulcer is a type of Peptic ulcer disease (PUD) — i.e., a sore (ulcer) in the lining of the upper small intestine (the duodenum) just beyond the stomach. (NCBI)
Specifically, it refers to a break in the mucosal lining of the duodenum, typically in the first part (often near the pylorus). (NCBI)
Duodenal ulcers are more common than gastric (stomach) ulcers in many settings. (Cleveland Clinic)
Epidemiology
-
Duodenal ulcers account for a large proportion of peptic ulcers (some sources say ~ 80 %). (Cleveland Clinic)
-
Occur across adult age groups; more common in 20-45 year age bracket historically. (NCBI)
-
Incidence has declined in many parts of the world owing to improved diagnosis and treatment of the underlying causes (e.g., H. pylori) and better NSAID monitoring. (NCBI)
Causes & Risk Factors
Primary causes
-
Helicobacter pylori (H. pylori) infection: A major factor. Many duodenal ulcers are associated with H. pylori colonisation/infection. (Patient)
-
Use of non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, aspirin: These can damage the protective mucous lining and make ulcer formation more likely. (Mayo Clinic)
Other contributing/risk factors
-
Smoking — delays healing, increases recurrence. (Hopkins Medicine)
-
Alcohol use and heavy drinking — may irritate mucosa and worsen symptoms (though they are less often the primary cause). (Patient)
-
Stress (especially physical stress such as serious illness) can contribute or worsen but is less likely a sole cause. (Cleveland Clinic)
-
Rare causes: Conditions that cause excess acid production (e.g., Zollinger‑Ellison syndrome), certain diseases (Crohn’s, malignancy), vascular insufficiency. (NIDDK)
Pathophysiology
-
Normally the duodenum has protective mechanisms (mucous layer, bicarbonate, epithelial integrity) that defend against stomach acid/pepsin. Ulceration occurs when the balance shifts: either increased acid/pepsin exposure or decreased protective capacity. (Patient)
-
H. pylori impairs mucosal defenses, causes inflammation, may increase acid secretion in some cases — resulting in damage. (NCBI)
-
NSAIDs inhibit prostaglandin synthesis which impairs mucosal blood flow, mucus & bicarbonate secretion, making mucosa more vulnerable.
-
Once the mucosa is damaged, acid/pepsin attack leads to ulcer formation.
Signs & Symptoms
Typical symptoms
-
Upper abdominal (epigastric) pain: often described as burning, gnawing or dull ache. (Cleveland Clinic)
-
In duodenal ulcers specifically: Pain often occurs when the stomach is empty, may wake the person at night, and may improve after eating or taking antacid. (Patient)
-
Other symptoms: bloating, belching, feeling full early after eating, nausea. (NIDDK)
-
Some people may have no symptoms until a complication occurs. (Cleveland Clinic)
Alarm/serious symptoms (indicating complications)
-
Vomiting blood (bright red or “coffee-ground” appearance)
-
Black/tarry stools (melena) or blood in stools
-
Sudden onset severe abdominal pain (possible perforation)
-
Signs of anemia (weakness, pale skin)
-
Unintentional weight loss, persistent vomiting, difficulty eating. (Healthdirect)
Diagnosis
-
History and physical examination: look for epigastric tenderness, risk factors (NSAID use, H. pylori risk)
-
Tests for H. pylori infection: urea breath test, stool antigen test, blood antibody test (though less preferable) (Hopkins Medicine)
-
Endoscopy (esophagogastroduodenoscopy, EGD): allows direct visualization of ulcer, location, size, and allows biopsy for H. pylori and rule out malignancy (especially for gastric ulcers) (NCBI)
-
Imaging (e.g., upper GI barium series) may be used if endoscopy is contraindicated or as an adjunct. (Hopkins Medicine)
-
Laboratory tests: For bleeding (CBC), liver/renal function, other causes.
-
Assessment of risk/complications: if bleeding, perforation suspected.
Treatment
Principles
-
Eliminate the cause (treat H. pylori if present; stop or modify NSAIDs)
-
Promote ulcer healing by suppressing acid, protecting mucosa
-
Lifestyle modifications to reduce aggravating factors
-
Monitor for and manage complications
Medications
-
If H. pylori positive: Combination therapy (usually 2 antibiotics + acid-suppressing agent) for eradication. (Hopkins Medicine)
-
Acid-suppressing drugs:
-
Proton pump inhibitors (PPIs) — e.g., omeprazole, pantoprazole
-
H2-receptor antagonists — e.g., ranitidine (though newer practice emphasises PPIs)
-
-
Mucosal protective agents: e.g., sucralfate, misoprostol (in some cases)
-
Antacids may relieve symptoms but are not sufficient alone.
-
If NSAIDs must be used, consider protective therapy (PPIs) concomitantly.
Lifestyle & supportive measures
-
Stop smoking
-
Limit alcohol intake
-
Avoid or reduce NSAIDs if possible; if necessary, use the lowest effective dose, for shortest duration, and consider protective agents. (Mayo Clinic)
-
Eat smaller meals, avoid foods that clearly trigger your symptoms (though diet alone doesn’t cause ulcers, but may aggravate)
-
Manage stress/physical stressors where relevant.
Duration & follow-up
-
Many ulcers heal in weeks (e.g., 4-8 weeks) with appropriate therapy. (Healthdirect)
-
After H. pylori treatment, it’s important to confirm eradication in many cases (via stool antigen or breath test).
-
If ulcer recurs or does not heal, further evaluation for complications or other causes is needed.
Complications
If untreated or severe, duodenal ulcers may lead to:
-
Bleeding: erosion into blood vessels → can cause hematemesis/melena, anemia. (Mayo Clinic)
-
Perforation: ulcer erodes fully through the duodenal wall → emergency with risk of peritonitis. (Healthdirect)
-
Gastric outlet obstruction: due to swelling/scarring near pylorus/duodenum → vomiting, weight loss, early satiety. (childrenshospital.org)
-
Recurrence: Without addressing underlying cause, ulcers may recur.
-
Rarely, malignant change (more relevant for gastric ulcers; duodenal less so) but still important to evaluate. (Mayo Clinic)
Prognosis
-
With modern treatment (H. pylori eradication + acid suppression), the healing rate is very good and recurrence rates are much reduced compared to older eras. (NCBI)
-
Prognosis worsens when complications occur (bleeding, perforation) or when underlying risk factors remain (continued NSAID use, smoking, untreated H. pylori).
Prevention
-
Avoid or minimise long-term/high-dose use of NSAIDs; use alternatives where possible, and if NSAIDs needed, use protective therapy (PPIs) and monitor. (NIDDK)
-
Eradicate H. pylori infection when detected (and treat associated family/contacts when indicated)
-
Stop smoking; limit alcohol; maintain healthy diet and weight
-
Good hygiene and sanitation: H. pylori transmission may be via oral-oral or fecal-oral routes (contaminated water/food). (NIDDK)
-
Manage stress or serious illnesses that may increase risk of ulceration (esp in hospitalised/ICU patients)
-
If you have risk factors (e.g., on NSAIDs, older age), have periodic evaluation and monitor for symptoms.
Special Considerations & Notes for India / Developing Countries
-
Prevalence of H. pylori is higher in many regions, which means screening may be more relevant.
-
Access to endoscopy may vary — treatment may sometimes proceed empirically based on clinical suspicion, though endoscopy remains gold standard for diagnosis and complications.
-
Nutritional status, hygiene, co-morbidities (e.g., tuberculosis, HIV, malnutrition) may modify presentation and risk; careful clinical evaluation is needed.
-
Cost/availability of PPIs, antibiotic regimens, and monitoring for H. pylori eradication may pose challenges; local guidelines and antibiotic resistance patterns should be considered.
When to Seek Medical Attention
Seek urgent medical help if you have:
-
Vomiting blood (bright red or ‘coffee-ground’ appearance)
-
Black, tarry stools or any visible blood in stool
-
Sudden, intense, worsening abdominal pain (possible perforation)
-
Unexplained weight loss, persistent vomiting, difficulty swallowing or eating
-
Signs of anemia (light-headedness, paleness, rapid heart rate)
(Patient)
Summary
A duodenal ulcer is a treatable but potentially serious condition. By identifying and treating the underlying cause (especially H. pylori, or eliminating risky NSAID use), suppressing acid, and making lifestyle modifications, most people heal well. Attention to complications, timely diagnosis, and follow-up are key.
If you like, I can pull up the latest Indian guidelines on management of duodenal/peptic ulcers, including recommended antibiotic regimens, local H. pylori resistance data, cost-effective treatments in India, and what to expect in the Indian healthcare context. Would you like that?
"This Content Sponsored by SBO Digital Marketing.
Mobile-Based Part-Time Job Opportunity by SBO!
Earn money online by doing simple content publishing and sharing tasks. Here's how:
- Job Type: Mobile-based part-time work
- Work Involves:
- Content publishing
- Content sharing on social media
- Time Required: As little as 1 hour a day
- Earnings: ₹300 or more daily
- Requirements:
- Active Facebook and Instagram account
- Basic knowledge of using mobile and social media
For more details:
WhatsApp your Name and Qualification to 9943990669
a.Online Part Time Jobs from Home
b.Work from Home Jobs Without Investment
c.Freelance Jobs Online for Students
d.Mobile Based Online Jobs
e.Daily Payment Online Jobs
Keyword & Tag: #OnlinePartTimeJob #WorkFromHome #EarnMoneyOnline #PartTimeJob #jobs #jobalerts #withoutinvestmentjob"

Comments
Post a Comment